Radiculopathy and Sciatica: Arm and Leg Pain
A model showing the cervical nerve roots as they leave the spinal column.
The signals that tell our arms and legs to move begin in our brains and travel down our spinal cord. In the neck and lower back, large bundles of nerve fibers called nerve roots leave the spinal cord at regular intervals - one for each bone in the spinal column. These nerve roots exit the spine and travel into the arms and legs, eventually innervating the muscles and supplying our strength and sensation.
When a nerve root is injured, compressed, or inflamed, it is called a radiculopathy. Radiculopathies can occur in the neck (cervical radiculopathy), or in the lower back (lumbosacral radiculopathy). Pain originates in the neck or back and shoots down the arm or leg. Often people suffering from radiculopathy have difficulty describing the pain: some call it lightning-like while others think of it as gnawing. It can come on slowly or worsen to excruciating levels. If the injury to the nerve root is severe enough, other neurologic signs such as numbness or weakness can occur.
Illustration showing spinal nerves in arms and legs.
Where a patient experiences pain depends on which nerve root is involved. We name the nerve roots for the level of the spina - C4, C5, etc. for cervical nerve roots and L4, L5, S1 for lumbar and sacral radiculopathies. By carefully listening to your history and performing a thorough neurologic exam, Dr. Hatef will determine which level is affected.
Although occasionally radiculopathy is caused by an underlying medical condition, the vast majority of cases involve mechanical compression from the spine. The nerves can be compressed or irritated by herniated discs, bone spurs, abnormal movements of the spine, or spinal arthritis. Although the history and physical exam will help identify the presence of radiculopathy, imaging studies with X-rays, CTs, and MRIs are required to pinpoint the cause of the compression.
This MRI scan shows a large disc herniation (arrow) that is compressing the nerve (seen in gray). This patient ultimately underwent arthroplasty.
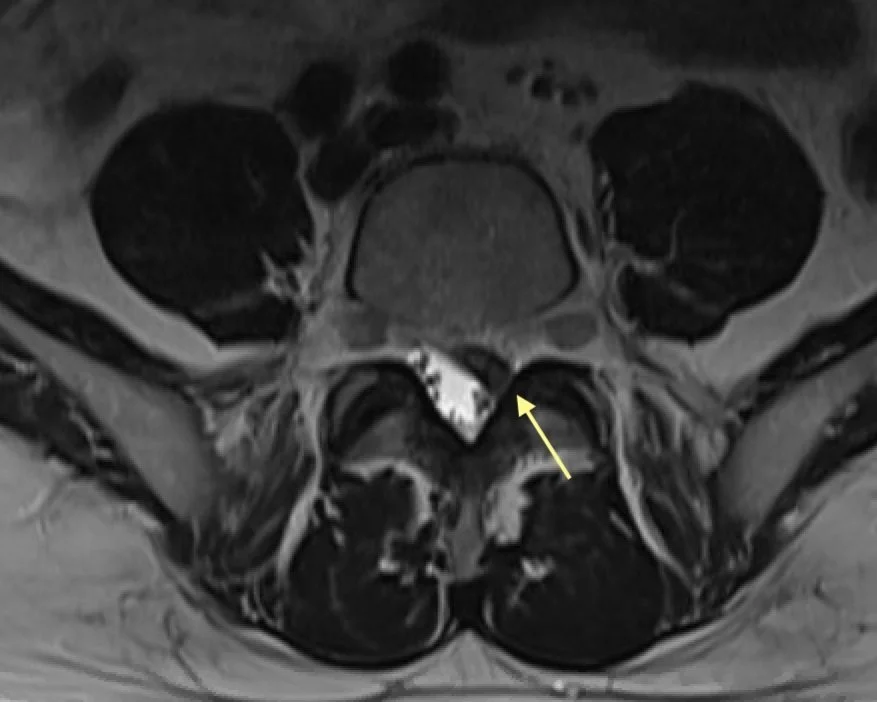
This MRI cross section of the lower back shows a large disc bulge (arrow) that is compressing the S1 nerve. This patient improved with conservative measures.
Most patients with radiculopathy will improve on their own, and disc herniations can heal on their own with enough time. The most important part of early management of radiculopathy is treatment with anti-inflammatory medications and physical therapy. Sometimes, patients can be candidates for epidural steroid injections (ESI) to try and directly bathe the nerve in anti-inflammatory steroids. Dr. Hatef believes that most patients will not need surgery and recommends a thorough trial of all nonoperative options before resorting to surgery on your spine.
For patients who fail to improve despite our best efforts, surgery is a very reasonable options. Most cases of radiculopathy can be treated with minimally invasive decompression techniques or arthroplasty. Dr. Hatef’s goal is to disrupt the normal condition of the spine as little as possible to quickly get you back to your normal life.