It’s just carpal tunnel, right?
You’re waking up at night with numbness. Or, you have tingling in your fingers when you write. And your wrist and hand hurt when you sleep.
Carpal tunnel syndrome is an extremely common diagnosis. In popular culture, it seems like carpal tunnel is mainly a joke - something that gives you grief when you spend all day at the computer. But in reality, carpal tunnel syndrome can be a painful or disabling diagnosis.
The carpal tunnel is a passageway between your forearm and hand. It’s called a tunnel because it’s completely enclosed by bone and ligaments. The bones of your wrist make a U-shaped container that is roofed by the transverse carpal ligament. Through this tunnel pass many important structures - the tendons for your fingers, arteries for your hand, and most importantly, the median nerve.
Illustration showing the muscles of the hand and the transverse carpal ligament. This structure is the roof of the carpal canal and is cut to decompress the median nerve in a carpal tunnel release.
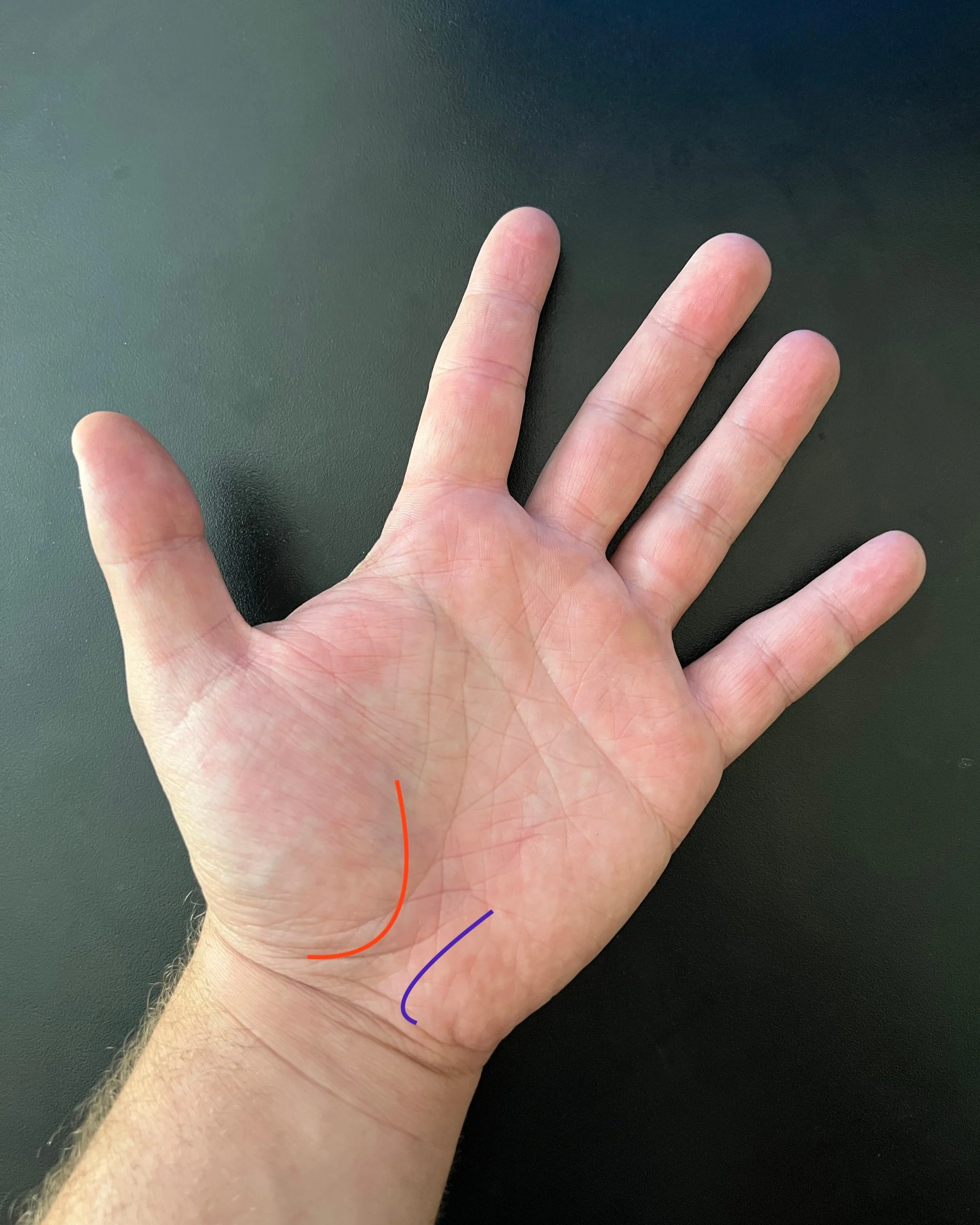
Photograph of a hand showing outlines or thenar (thumb muscles - red) and hypothenar (small finger muscles - blue). Between the two muscle masses lies the carpal canal.
In most people, there is plenty of space inside this carpal tunnel. All the structures can smoothly glide past one another without being compressed or irritated. Carpal tunnel syndrome begins when the space in the tunnel becomes limited. As the tunnel becomes less spacious, the median nerve is the first structure to become irritated because it is the most susceptible to any compression.
In most people, carpal tunnel syndrome is a condition caused by age; however, there are instances where it is caused by a specific, structural problem. There can rarely be tumors or cysts of the tunnel, and in young women during pregnancy, the swelling that occurs throughout the body leads to narrowing of the tunnel as well. Despite these rarer conditions, the most typical reason for carpal tunnel syndrome is age-related. As we get older, there are wear and tear changes throughout our bodies, leading to arthritis of our joints, and in some patients, narrowing of the carpal tunnel.
Symptoms
What are the main symptoms of carpal tunnel syndrome? How do you know if you have it? The symptoms of carpal tunnel syndrome all relate to the functions of the median nerve. After it passes through the carpel canal, the median nerve branches into multiple smaller nerves to supply its final functions. It has two main jobs - supplying sensation for the thumb, index, and middle finger, and supplying the motor function, or strength, for the large muscles of the thumb. So, when the median nerve is compressed, any of these major functions can be impaired.
Numbness in carpal tunnel syndrome. The dots were drawn according to where the patient felt numbness and tingling. Note that the thumb, index, middle, and half of the ring finger are involved.
Typically, pain is the earliest symptom. Anytime a nerve is injured, there can be pain. Often, the pain is felt it in the distribution of the median nerve – the thumb, index, and middle finger. However, in some patients the pain is vague, only being felt in the palm or wrist.
If the condition progresses, numbness or weakness can occur. All of the symptoms seem to be worse at night. Often, when we sleep, our hands and wrists end up flexed into uncomfortable positions that worsen any compression on the median nerve. And sometimes when we sleep, the amount of swelling in our tissues increases. Everyone has had the feeling that their hands or feet are a little bit more swollen in the mornings, and usually this doesn’t cause any real concerns. However, in someone with compression in the carpal canal, this small amount of additional swelling can be enough to cause symptoms at night.
There are two common ways to diagnose carpal tunnel syndrome: the neurologic exam and nerve conduction studies. When you see your family doctor, neurologist, or neurosurgeon, he or she starts with a history and physical – usually the symptoms of carpal tunnel syndrome are so characteristic that diagnosis can be made then. When doctors examine your hand, we can often identify that the sensation in your hand is decreased in the area supplied by the median nerve, supporting this diagnosis. However, in many cases, nerve conduction studies are ordered.
A nerve study allows us to diagnose carpal tunnel syndrome and also determine how severe each case is. When a nerve first becomes compressed, often there is a lack of blood flow. This happens to nearly everyone at some point in life - waking up at night with some numbness in the hand or arm because of an awkward sleeping position. With further progression, the nerves themselves become injured - first the lining of the nerves (similar to insulation on an electrical cable), and eventually the nerve itself. The nerve study, performed by a neurologist, allows us to determine to what stage the syndrome has progressed. This has two main benefits - it gives us an idea of how bad things are, and it gives us an idea of how quickly things will get better.
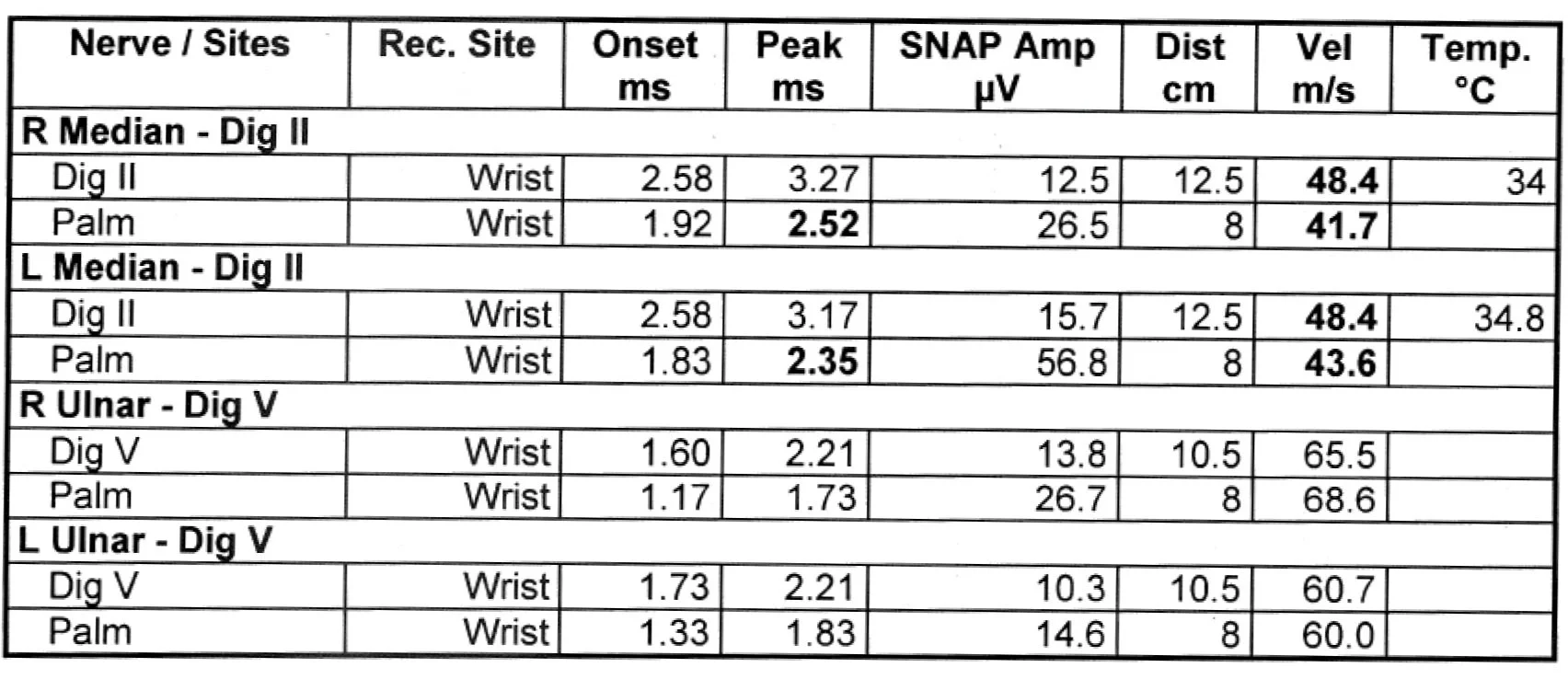
Nerve study showing carpal tunnel syndrome. The abnormal results are in bold. Compared to the normal ulnar nerves, the velocity (nerve conductions speed) is slower and the amplitudes are lower (showing fewer nerve fibers firing). Overall, this patient had moderate carpal tunnel syndrome and improved after surgery.
Treatments
So, what are the treatment options for carpal tunnel syndrome? There are two general treatments - surgery and conservative measures. For patients with severe symptoms that are interfering with life, or those with very severe changes on the nerve study, we usually recommend surgery. However, most people come in with more mild symptoms. In those cases, surgery is not needed initially, and can hopefully be avoided. Wearing a wrist splint at night helps prevent awkward positions when you sleep and eases the compression of the median nerve often.
Cross-section of a hand showing the carpal canal, median nerve (in center, yellow) and transverse carpal ligament (colored blue). The ligament is cut to open the carpal canal and decompress the median nerve.
Injection of steroids can also be applied near the nerve. Steroids decrease inflammation, and when injected onto the nerve surface they can reverse some of the changes of mild compression. Some patients come in with mild symptoms that respond well to a brace and injections, while others continue to progress. We don’t exactly know why this is the case, and this is why we usually recommend that everyone try non-operative measures before going to surgery.
Surgery for carpal tunnel syndrome is nerve decompression surgery. The main structure that we look to cut during surgery is the transverse carpal ligament – the “roof” that turns the carpal tunnel into a fully enclosed space. When we cut this, it opens the canal and releases the compression on the median nerve.
Although this is a simple operation, the stakes are obviously high. Hand function, especially in the dominant hand, is one of the most important parts of our bodies. By remaining slow and deliberate, surgeons send identify and cut the transverse carpal ligament without injuring any important motor or sensory fibers from the median nerve.
Outcomes
When will I get better? Will I get better? Should I have this done?
These are obviously patients first questions and the most important questions. And, for most patients, carpal tunnel syndrome does not cause severe impairment of sensation or strength, only intermittent pain or numbness. For these patients, excellent recovery is expected, with symptoms improving nearly immediately. People can usually tolerate light work by 2 to 3 weeks, and return to heavier labor after 6 to 8 weeks. The incision is small and the recovery complete. For patients with more severe symptoms, such as severe numbness or weakness of the thumb muscles, it is a little bit more difficult to determine the prognosis. The nerve studies are very helpful in this regard. Nearly all patients improve, but if there is severe damage to the nerve fibers identified on the nerve studies, some of the symptoms may be permanent. Thankfully, this is very uncommon in carpal tunnel syndrome, since it is so common and quickly recognized.
Carpal tunnel decompression surgery. The transverse carpal ligament has been cut. The median nerve is seen below it, and it is darker than usual due to the prolonged compression.
Photograph showing scar appearance after about two months. The scar will continue to lighten over 1-2 years.
What should you do if you think you have carpal tunnel syndrome? The first step is obviously to see your primary or family doctor, but should you see a surgeon to discuss decompressive surgery? I am a firm believer that the best time to meet a surgeon and discuss your condition is before you need surgery. The best conversations I have with patients are when their symptoms are mild. We can discuss the symptoms, the reasons for the condition, and the non-operative measures people can try to get relief. And during this conversation, there is minimal pressure, since the symptoms are mild and most people aren’t contemplating surgery anyway. I’ve found that patients leave these conversations satisfied with a plan and knowledge of what kinds of symptoms to look out for. Many patients don’t return. They never need surgery. And for those patients that do need surgery, they have a relationship with me and know to call when things change. It’s always more stressful to have a discussion with a surgeon when symptoms are bad, or worse, when symptoms are so severe that you know you need surgery. This is why I always welcome at patients to see me even if they think they might not need surgery, or even if they know they don’t need surgery.
Carpal tunnel syndrome is a very treatable condition. If you think you may have it, get seen soon. Don’t let things progress until nerve damage occurs. Despite what TV and movies may have you believe, it’s not just carpal tunnel.