The minimally invasive approach
Steve was a 52-year-old man who came to the office with severe back and leg pain. It had been going on for about nine months. He was a welder, constantly on his feet and crouching throughout the day, and as the pain had escalated, he had been having a lot of trouble completing his work. He was even considering reducing his hours. He tried physical therapy, water therapy, chiropractic manipulations, and injections, but nothing seemed to help. We ordered an MRI which showed severe degenerative disc disease at the L4-L5 level. There was compression of the spinal nerves, both in the central spinal canal and in the foramen where they exit into the body before coursing into the legs.
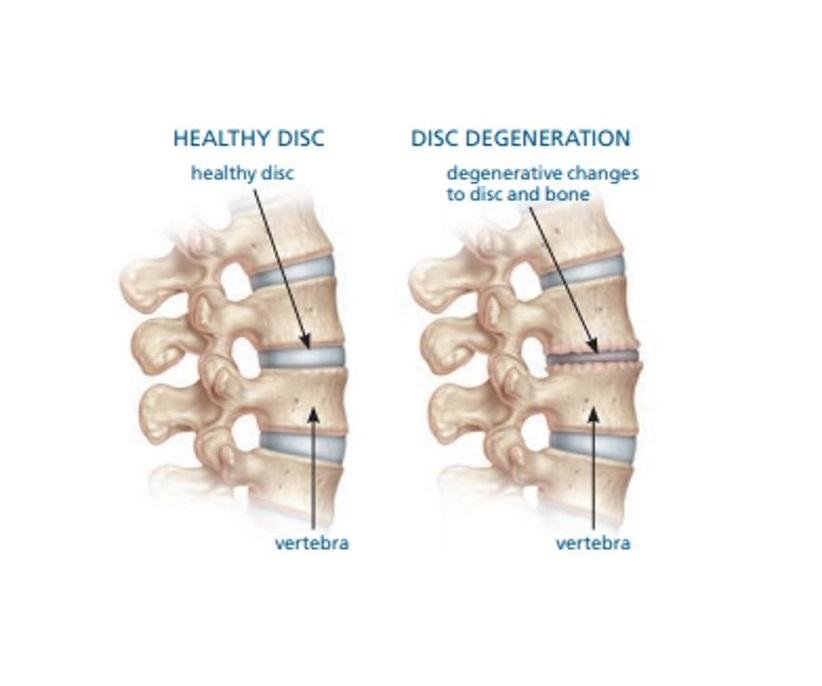
Degenerative disc disease is a form of spinal arthritis. As the arthritis progresses, there can be impingement and compression of the spinal nerves.
He was determined to rehabilitate as quickly as possible after surgery. We treated his compression with a minimally invasive lumbar fusion. In this case, it was a transforaminal lumbar interbody fusion – TLIF. He was able to get out of bed and walk the first day after surgery, and even though he was sore, he went home from the hospital about 36 hours after his surgery. He was in physical therapy for light exercise within about four weeks, and he was back to work full-time on light duty at six weeks.
What about his surgery was different from a traditional lumbar fusion? How can we improve on open surgery?
Minimally invasive surgery
Minimally invasive surgery is a broad category. Depending on the specialty, it can have different meanings. One of the earliest specialties to adopt minimally invasive surgery was general surgery. Many people know individuals that had traditional, open procedures for abdominal procedures decades ago. It’s not uncommon to see incision along the whole length of the rib cage for someone who had their gallbladder removed in the 1980s or 1990s. But the development of specialized cameras - laparoscopes - led general surgeons to offer minimally invasive techniques that involved small incisions. Using this advanced technology, they were able to perform many operations using cameras and narrow instruments as opposed to having a traditional, open approach. It is now uncommon to have an open procedure to remove a gallbladder. All of this has led to dramatically improve rates of blood loss, hospital state, and pain after surgery.
But, can the same thing be done in spine surgery.
Minimally invasive surgery for the spine is different in a number of ways. Unlike the abdomen, there is no “cavity” into which cameras can be introduced. The muscles of the back and neck adhere strongly to the vertebrae and can impede access. And, the reasons for spine surgery are different as well. During spine surgery, we are typically not removing organs, we are decompressing nerves. Can these decompression procedures be safely performed with technological advances, even though direct visualization is limited?
The tubular approach
In a traditional, open approach, a long incision is made in the middle of the back. The paraspinous muscles, the strong muscle groups found on either side of the spine, are removed from the vertebrae to be operated on and retracted to the side. This allows the surgeon to have visualization of the entire vertebrae from side to side.
Photograph of dilation tubes. These small tubes are inserted directly through the muscle with minimal damage. An intraoperative microscope is used to perform surgery through the small opening.
Most minimally invasive procedures in the spine rely on a technology called dilation tubes. A minimally invasive approach using a tubular retractor is quite different from an open procedure. A small incision is made on the side of the spine, anywhere from 1 to 4 cm from the midline. Then a series of hollow cylinders are advanced through the muscle. These cylinders, commonly called tubes in spine surgery, are used to spread the muscle fibers and provide exposure of the vertebrae. This allows for exposure of the spine through a very small incision – for a simple decompression procedure, the incision may be as small as 2 cm. Surgeons use operative microscopes to see down the narrow tubes and specialized microsurgical instruments to work in narrow spaces.
Intraoperative X-ray showing small 2cm tube (left) used to make approach. Also seen is an example of the microsurgical instruments used in minimally invasive surgery.
The tubular approach has a number of advantages. Because the approach is directly through the muscle, the procedure preserves the midline of the spine. In the midline of the spine are the spinous processes. In most people they can be felt just beneath the skin in the middle of the spine. These are long, strong bony extensions of the vertebra that provide attachments to the paraspinal muscles and ligaments. Traditional spinal surgery detaches the muscles from the spine. But, unlike a large muscle such as the biceps or pectoralis muscle that can be reattached at the end of surgery, the paraspinal muscles are too small to directly reattach to the bones at the end of surgery. Healing relies on the formation of scar tissue to reattach the muscles to the spine. An approach off the midline, known as a paramedian approach, avoids detaching the muscles from the spine. Spreading the muscles fibers does injure them slightly, but it is much easier for the body to heal from this small injury compared to larger open procedures.
Using a tubular retraction system allows for a smaller approach. The nearby photograph is a cross-section of the spine in a patient with compression of the nerves. The arrow shows the trajectory used to access the intravertebral disc – this is the main target for both micro discectomy decompression procedures, and TLIF lumbar fusion procedures. The minimally invasive approach allows us to take a direct path to our target and avoid collateral damage to normal muscle tissue. This allows for a much smaller incision.
MRI image showing disc herniation (yellow). The minimally invasive approach is show in pink. An approach through the muscle minimizes damage and is the shortest and most direct trajectory to the spine.
Increased stability
There is one more advantage to a minimally invasive procedure. In the midline of the spine, the spinous processes are not isolated by themselves. They are connected to one another by strong ligaments – the interspinous and supraspinous ligament. These ligaments are thought to be one of the main stabilizers of spinal motion. During a traditional approach, these ligaments are injured, first by the detachment of the muscles, and then by the removal of the bones and spinous processes. However, a paramedian approach avoid these damaging effects on the ligaments. Preserving these ligaments helps prevent spinal instability.
Illustration of the spinous processes and associated ligaments. These midline structures provide stability to the spine and are at risk of injury during open approaches. Minimally invasive approaches try to avoid these ligaments and preserve stability.
Stability of the spine is a broad term. On one extreme, is a completely healthy spine in a young person. There has been no injury to any bones, muscles, or ligaments, and the wear-and-tear changes of life have not led to any arthritis yet. This individual’s spine is stable. The other extreme is a patient’s spine after a severe car accident. There can be total destruction of bones and ligaments, and without immediate surgery, this patient is likely to develop severe neurologic problems. This patient has an unstable spine.
The instability after open surgery is different. Imagine a procedure for spinal fusion done in an open fashion. The muscles are moved aside, and all of the organs that help stabilize motion are exposed – the ligaments, the strong joint capsules surrounding joints, and the muscles themselves. These stabilizing structures can easily be injured during the course of this procedure. Spine surgeons strive to preserve all of the important natural stabilizers of the spine, but sometimes that is impossible and small injuries occur in the ligaments. If there is any small damage to some of the ligaments and capsules, this might be to development of instability.
Using a minimally invasive approach avoids exposing all of the normal structures of the spine. By using minimally invasive techniques, neurosurgeons can expose only what is necessary to decompress the nerves and avoid collateral damage to these normal structures.
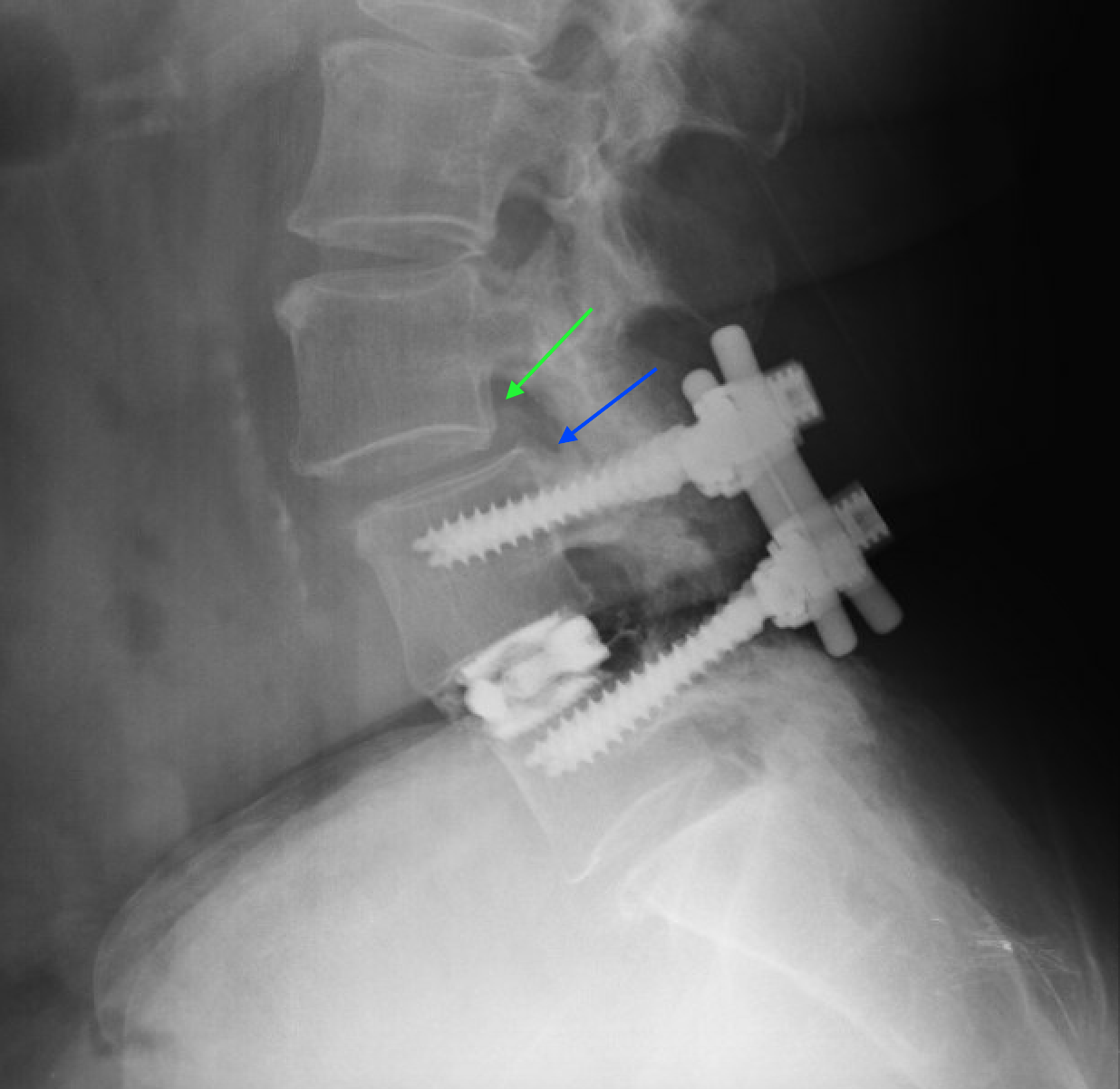
Adjacent level degeneration. Postoperative X-ray 4 years after open lumbar fusion at the L4/5 level. There is degeneration of the L3/4 level above the screws. There is also slippage of the L3 vertebra (green) compared to the L4 vertebra (blue). Injury to the stabilizing structures can lead to long-term degeneration and future surgery. Minimally invasive techniques attempt to limit damage.
But, what does this instability look like? In most cases, patients recover well from surgery – open or minimally invasive – and get back to their normal life. But the micro-damage that was done during surgery weakens the stabilizing structures. This can lead to abnormal movements and the development of arthritis at nearby levels. This is called adjacent segment degeneration. For example, during our L4-L5 lumbar fusion, what if we damage the structures that stabilize the L4 vertebrae to the L3 vertebrae? Our patient would recover from surgery and rehabilitate. But there is a possibility that by damaging those ligaments, we have hastened the development of arthritis at the L3-L4 level. These effects can lead to the need for surgery at other levels in the future.
One of the goals of minimally invasive surgery with a tubular retractor system is to avoid this collateral damage. By limiting our exposure to a small area of bone – just big enough to complete our decompression and fusion procedures – we prevent injury to these nearby structures. The hope is that we can improve the long-term stability of the other spinal levels and prevent the development of arthritis requiring more surgery.
Am I a candidate?
Minimally invasive surgery has limitations, and open surgery does have advantages. The most important advantage in open surgery is the ability to achieve fusion.
A TLIF procedure. The diseases disc has been replaced with bone graft and spacers to promote fusion in the front of the spine, between the “bodies” of the vertebra. This procedure can be done open or minimally invasively.
Fusion is the joining of two bones into one. With a combination of hardware and techniques such as bone graft, two nearby bones can be joined together to form one solid piece of bone. However, in order for this to happen, there must be a scaffold between the two bones for new bone to grow. During an open procedure, this is not a problem. The muscles have been moved aside and a surgeon can lay down as much scaffold as he or she thinks is needed to promote fusion. However, in minimally invasive surgery, the muscles are left attached to the bones. There is limited ability to place bone graft to promote fusion.
If the ability for fusion is so limited, how can we perform fusion surgeries minimally invasively? The most common way to achieve fusion minimally invasively is through interbody fusion. As the name implies, the fusion occurs between the two “bodies” of the vertebrae – the part of the vertebrae found in front of the spinal nerves. Interbody fusion can be achieved through a variety of approaches, but one of the most common approaches for a minimally invasive fusion is the minimally invasive TLIF. This allows the surgeon to get past the nerves and into the intervertebral disc, remove the disc, and place bone graphs and spacers into the disk space that promote fusion between the two bodies.
Minimally invasive TLIF has excellent rates of fusion. There is ample blood supply to the vertebral bodies – a necessary ingredient for fusion – and fusion rates in minimally invasive TLIF are comparable to traditional approaches. But this surgery does illustrate one of the main limitations of minimally invasive surgery. It is perfectly acceptable to perform interbody fusion at one, two, or even three levels – but what about a patient with scoliosis who requires fusion of many levels? Or, what about a patient whose neural anatomy does not allow for minimally invasive TLIF? In these cases, to attempt a minimally invasive approach may result in decreased rates of fusion.
This also limits our utilization of minimally invasive approaches in trauma. In most traumatic cases, the injury occurs not only through the bones, but also through the joints and ligaments connecting the bones, causing instability. In these cases, we rely on fusion to achieve long-term stability, as the spinal ligaments do not heal reliably. This makes minimally invasive approaches to severe trauma difficult. Because fusion is necessary for a good result, we often must resort to open approaches in these injuries.
Is it worth it?
Minimally invasive surgery of the spine has not caught on with nearly the same popularity as minimally invasive abdominal surgery. Many surgeons think it is too cumbersome, or think the patients who are candidates are too rare. The traditionalists do have a point: open surgery is reliable, time tested, and despite somewhat more pain and blood loss, people recover well by 6 to 8 weeks.
So, why do minimally invasive spine surgery? I think it comes down to a philosophy of surgery. Yes, the end results are not that different – less blood loss, slightly smaller incisions, and fewer days in the hospital. But if a surgeon performs hundreds, or even thousands, of these procedures, by using minimally invasive approaches whenever possible, he or she can improve the pain and quality of life for patients. At the two-year follow up, patients treated with open or minimally invasive techniques have similar outcomes. But, why not improve things as much as possible during those first two years?